For some families, getting pregnant can be a challenge. That challenge may lead them to consider in vitro fertilization, or IVF. “In vitro,” by the way, means “in glass” in Latin.
With IVF, doctors collect eggs and sperm and do the fertilization themselves outside of the body. The resulting embryo is cultured and then transferred into the woman’s uterus. This process, while easy to describe, is incredibly complex and difficult. Embryo transfer is hard, and not every embryo that’s successfully transferred leads to a healthy pregnancy.
So, families often wind up paying for multiple cycles of IVF. At somewhere between $10,000 and $15,000 per cycle, the process can easily approach $50,000 for a pregnancy to occur. That’s too expensive for many families.
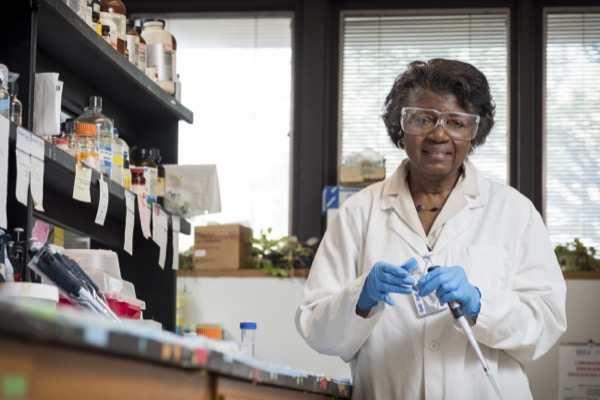
Recently, Patricia DeLeon, a professor of biological sciences at the University of Delaware, was awarded a grant from the Delaware Bioscience Center for Advanced Technology (CAT). That grant would help her, through a partnership with the Reproductive Associates of Delaware (RAD), develop a non-invasive way to identify embryos with the best chance at resulting in a healthy pregnancy for parents seeking IVF. That could potentially make it so that patients only need one cycle of IVF to get pregnant, not three.
DeLeon took time to speak with us about the grant and her work. When our conversation started, she proudly told us, “I’ve just begun my 41st year at UD. I came in 1976.”
The Bioscience CAT grant was awarded to six different projects and partners earlier this year. The program’s goal is to further foster Delaware’s growth in the bioscience field, something everyone we’ve spoken to so far for this story has reinforced. It seems that its potential influence on the state, country and world is huge.

Delaware Biotechnology Institute, home of the Bioscience CAT. (Courtesy photo)
“This is the first time I applied for the grant,” DeLeon told us. “It’s been here for five years? Six years? You have to have a partner, and we’ve been in association with RAD for a long while. We’ve been working on, sort of, the sperm part rather than the embryo part, which really is the more interesting of the two.”
That more interesting part, the bit with the embryo? That’s what the Bioscience CAT grant will help fund. For DeLeon and RAD, the grant means funding to make the IVF process even better.
“The problem we have right now is not so much getting the sperm to fertilize the egg, but it’s getting the embryo to implant and develop. For in vitro fertilization, you can get the sperm and the egg together in a dish. You can put them together. If the sperm is even lazy and can’t swim, you can do the swimming for them so they can fertilize.”
A Delaware fertility center has the best single-embryo transfer success rate in the nation: 95.6 percent.
But implanting that into the uterus: “That seems to be the roadblock,” she told us. “That’s where the success is lacking right now.”
When we asked DeLeon about current success rates, she was understandably hesitant to give me a number. “If you go to the CDC, the CDC says 30 to 32 percent success rate across for IVF, right? But that data is kind of hard to tease out. If you go to England or Europe, they’ll say 30 percent. It’s so hard to tease out because it’s a composite rate. It includes mothers who are much older who are producing eggs that are not so good. If you get to the embryo stage, I’d say it’s closer to 50 percent. Generally, though, the rate across the board is going to be stated as 30 percent.”
“That’s why most couples have to undergo three cycles of IVF before they get it right,” she said. “It’s expensive. It’s tough even to make it available to people who are not very wealthy.”
“My goal,” DeLeon went on, “is to come down to the point where you can select a single embryo and have that single embryo produce a healthy child.”
Which would be enormous. Transferring multiple embryos may increase the potential for pregnancy, but it also introduces lots of risk. The most obvious among them is twin pregnancies. Single embryo transfer is desirable.
DeLeon pointed us to a story by Forbes that cited RAD as having the best single-embryo transfer percentage in the nation: 95.6 percent. The next closest organization was the Fertility Centers of New England, with a transfer rate of 79.3 percent.
“We have one outlet [RAD] that’s top of the nation in doing what really should be done: that’s single embryo transfer,” DeLeon explained.

This is an 8-cell embryo at three days. (Photo from the RWJMS IVF Program, via Wikimedia Commons)
DeLeon told us that you can transfer only one embryo to the uterus, but that really only stands a roughly 50 percent chance of developing into a healthy child. Her goal is to develop a non-invasive way to identify embryos that will have a much stronger chance of developing.
“What happens is that they have to stick to the womb, to the lining of the endometrium. It’s the implanting, the getting itself into the lining of the uterus that is important. If they don’t get implanted, they won’t develop.”
Let’s talk about the invasive, contemporary method of determining an embryo’s viability first. As DeLeon explains it, doctors gather eggs and sperm. They make fertilization happen in a dish. The fertilized egg develops into a blastocyst, which is a phase before the early embryo. With this current method, doctors actually stick a needle into the blastocyst to remove a cell to determine future embryo viability. That’s the invasive bit that’s causing potential unnecessary damage.
With DeLeon’s method, the blastocyst releases tiny vesicles. These tiny particles, as she put it in lay for us, carry cargo. That “cargo” consists of proteins, RNA and even DNA. Instead of putting a needle into the cell, the non-invasive method DeLeon and RAD are after involves looking at those tiny particles to determine viability and select the best embryo.
If DeLeon and RAD’s work pans out, families that wouldn’t be able to afford the potentially costly IVF procedure will only need one cycle instead of possibly three. That’s $10,000-$15,000 instead of $30,000-$45,000.
“The first time you go, not only will the embryo stick, but it will be a healthy embryo.”
Think about what that new potential affordability means for families looking to conceive and deliver a healthy baby. This could be huge.
DeLeon asked parents of successful IVF pregnancies or those looking to support the cause consider looking to the University of Delaware Family Building Research Fund. Find more information about that here.
Join the conversation!
Find news, events, jobs and people who share your interests on Technical.ly's open community Slack

Delaware daily roundup: Delmarva Power vendor stats; DelDOT's $15M federal grant; 50 best companies to work for

Delaware daily roundup: Over 4,000 Black-owned businesses uncovered; Dover makes rising cities list; a push for online sports betting

Delaware daily roundup: Ladybug Fest illuminates small biz; Hahnemann Hospital's biotech future; intl. politics and a Middletown project